The trochlear nerve, also known as the fourth cranial nerve, plays a crucial role in eye movement. When this nerve is damaged, it can lead to various symptoms and complications that can significantly impact an individual’s vision and quality of life. In this article, we will explore the anatomy and function of the trochlear nerve, the causes of its damage, the symptoms associated with such damage, the diagnostic process, available treatment options, prognosis, and recovery, as well as the overall impact on daily life and available support resources.
Understanding the Trochlear Nerve
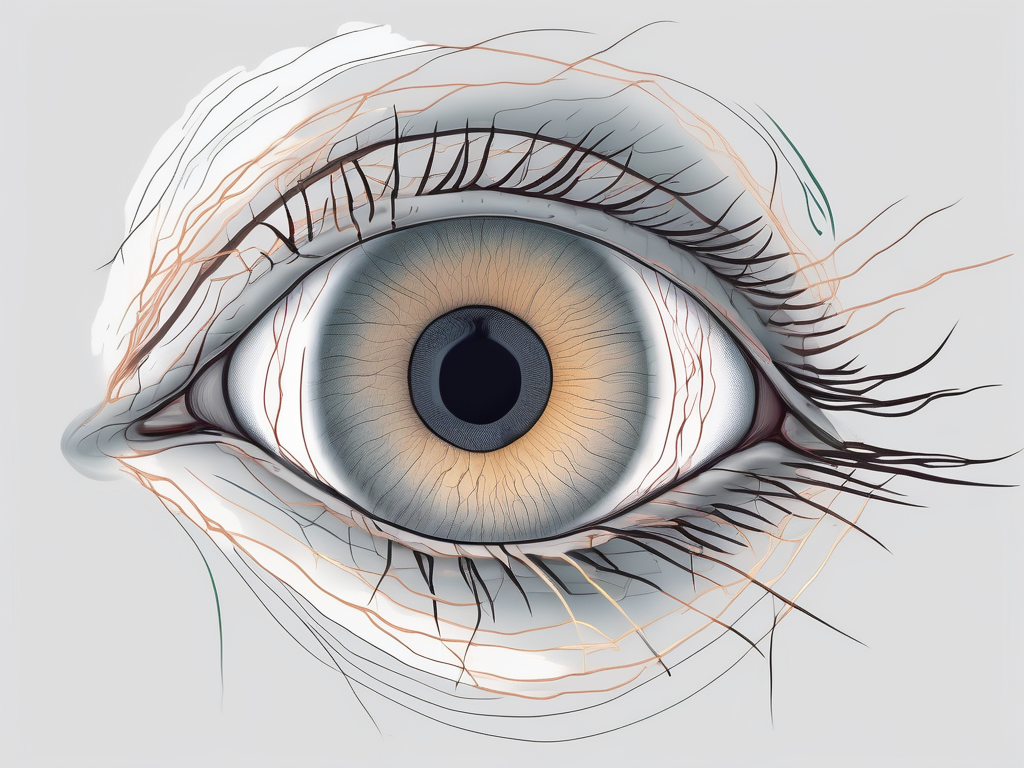
Anatomy of the Trochlear Nerve
The trochlear nerve, also known as the fourth cranial nerve, emerges from the brainstem and is the only cranial nerve that exits the dorsal aspect of the brainstem. It originates from the trochlear nucleus, located in the midbrain, and travels along a complex pathway to reach its target muscle.
The trochlear nerve primarily innervates the superior oblique muscle, one of the six extraocular muscles responsible for eye movement. The superior oblique muscle aids in downward and inward eye movement, allowing us to look down and towards the midline. This muscle is unique in its orientation and function, as it is the only muscle that pulls the eye in a direction opposite to its line of action.
Unlike other cranial nerves, the trochlear nerve crosses over and innervates the contralateral eye. This means that the nerve from the left side of the brainstem controls the right superior oblique muscle, and vice versa. This unique anatomical arrangement allows for coordinated eye movements and binocular vision.
Due to its long intracranial course and close proximity to the tentorium cerebelli, the trochlear nerve is susceptible to certain types of damage. Any injury or compression along its pathway can result in trochlear nerve palsy, leading to impaired eye movements and visual disturbances.
Function of the Trochlear Nerve
The trochlear nerve plays a crucial role in coordinating eye movements, especially when looking downward and inward. When we look down, the superior oblique muscle contracts, causing the eye to rotate downward and outward. This movement is essential for tasks such as reading, walking downstairs, and navigating our environment.
Additionally, the trochlear nerve contributes to the fine-tuning of eye movements during convergence, which is the ability of the eyes to turn inward to focus on nearby objects. This coordination ensures that both eyes are aligned and working together to provide a clear and single image.
When the trochlear nerve is damaged, these coordinated movements become impaired, leading to a range of symptoms and visual disturbances. Trochlear nerve palsy can result in vertical diplopia, which is double vision in the vertical plane. This means that when looking downward, the affected eye may deviate inward or outward, causing a misalignment of the images seen by each eye.
In addition to double vision, individuals with trochlear nerve palsy may experience difficulty with tasks that require looking downward, such as reading, writing, and using stairs. They may also have problems with depth perception and may tilt their head to compensate for the misalignment of the eyes.
Understanding the anatomy and function of the trochlear nerve is crucial in diagnosing and managing conditions that affect its integrity. By identifying and addressing any issues with this unique cranial nerve, healthcare professionals can help patients regain optimal eye movements and visual function.
Causes of Trochlear Nerve Damage
The trochlear nerve, also known as the fourth cranial nerve, plays a crucial role in eye movement. Damage to this nerve can result in various visual disturbances and impairments. While the causes of trochlear nerve damage can vary, there are several common factors that can lead to its impairment.
Trauma and Injury
Trauma and injury, particularly to the head or eye socket, can cause damage to the trochlear nerve. This can result from falls, sports-related accidents, motor vehicle collisions, or any situation that involves a direct blow to the head or eye region. The forceful impact can disrupt the delicate structures surrounding the nerve, leading to its dysfunction.
It is important to note that the severity of trochlear nerve damage can vary depending on the extent of the trauma. Mild cases may only result in temporary impairment, while severe injuries can lead to long-term or permanent visual deficits. Prompt medical attention is crucial in such cases to assess the extent of the damage and provide appropriate treatment.
Neurological Disorders
Certain neurological disorders can also lead to trochlear nerve damage. Conditions such as multiple sclerosis or tumors affecting the brainstem or the vicinity of the trochlear nerve can result in its impairment. These disorders may cause the compression or demyelination of the nerve, disrupting its normal function.
Diagnosing trochlear nerve damage in the context of neurological disorders can be challenging. It requires a comprehensive evaluation by a neurologist or a healthcare professional experienced in neurological disorders. Accurate diagnosis is essential for appropriate management and treatment of the underlying condition.
Surgical Complications
In some cases, surgical procedures involving the eye or brain can inadvertently damage the trochlear nerve. This can occur when there is accidental nerve injury during delicate surgical maneuvers or due to the surgical removal of tumors or anomalies in the region. Surgeons must exercise caution and employ meticulous techniques to minimize the risk of damaging the trochlear nerve during these procedures.
Preventing trochlear nerve damage during surgery requires a thorough understanding of the nerve’s anatomy and its relationship to surrounding structures. Surgeons must carefully plan their approach and take necessary precautions to avoid any inadvertent injury to the trochlear nerve. In complex cases, the involvement of a multidisciplinary team, including neurosurgeons and ophthalmologists, may be necessary to ensure the best possible outcome.
It is important to note that trochlear nerve damage caused by surgical complications can have significant implications for the patient’s visual function. Rehabilitation and specialized care may be required to optimize visual outcomes and improve the patient’s quality of life.
Overall, understanding the causes of trochlear nerve damage is crucial in preventing and managing this condition. Whether it is trauma, neurological disorders, or surgical complications, prompt diagnosis and appropriate treatment are essential for the best possible outcomes. It is important for individuals to seek medical attention if they experience any visual disturbances or symptoms that may indicate trochlear nerve damage.
Symptoms of Trochlear Nerve Damage
Trochlear nerve damage can have a range of symptoms that can significantly impact an individual’s vision and daily activities. In addition to the commonly experienced visual disturbances, there are other notable symptoms that may occur.
Visual Disturbances
Trochlear nerve damage can cause visual disturbances, including double vision (diplopia) or blurred vision. The affected individual may experience difficulty focusing on objects, especially when looking downward or inward. These visual abnormalities can significantly impact one’s daily activities, such as reading, driving, or even recognizing faces.
Double vision, also known as diplopia, occurs when the eyes are unable to align properly, resulting in the perception of two images instead of one. This can be particularly disorienting and can make it challenging to navigate the world. Blurred vision, on the other hand, can make objects appear fuzzy or out of focus, making it difficult to see details clearly.
Eye Movement Disorders
Impaired eye movements are a hallmark of trochlear nerve damage. The affected individual may have difficulty moving their eye downward or inward, leading to limited or restricted eye mobility. This can affect eye coordination and alignment, leading to a misalignment of the eyes (strabismus) or crossed eyes (esotropia).
Eye movement disorders can have a significant impact on an individual’s ability to track objects or follow a moving target. This can make activities such as reading, playing sports, or even watching television challenging and frustrating. The misalignment of the eyes can also affect depth perception, making it difficult to accurately judge distances.
Pain and Discomfort
Sometimes, trochlear nerve damage can be associated with pain or discomfort around the eye or forehead region. This pain can be mild to severe and may worsen with eye movements or when exerting the eye muscles. It is important to consult with a healthcare professional to determine the underlying cause of such pain and to explore appropriate management strategies.
The pain and discomfort experienced with trochlear nerve damage can vary from person to person. Some individuals may only experience mild discomfort, while others may have more severe pain that interferes with their daily activities. It is crucial to seek medical attention to determine the cause of the pain and to develop a personalized treatment plan.
In conclusion, trochlear nerve damage can manifest in various ways, including visual disturbances, eye movement disorders, and pain or discomfort. These symptoms can significantly impact an individual’s quality of life and should be addressed with the help of healthcare professionals. Early diagnosis and appropriate management strategies can help alleviate the symptoms and improve overall visual function.
Diagnosis of Trochlear Nerve Damage
When it comes to diagnosing trochlear nerve damage, a thorough clinical examination is absolutely crucial. This examination is typically conducted by a healthcare professional who specializes in neurology or ophthalmology. During the examination, the healthcare professional will carefully assess various aspects of the patient’s eye function to determine if there are any signs of trochlear nerve damage.
One of the key areas that the healthcare professional will focus on is eye movements. They will observe how well the patient is able to move their eyes in different directions, paying close attention to any abnormalities or limitations. In addition, they will also assess eye coordination, looking for any signs of misalignment or difficulty in focusing.
Visual acuity is another important factor that will be evaluated during the clinical examination. The healthcare professional will test the patient’s ability to see clearly at different distances, using various charts and tools. This helps to determine if there are any vision problems that may be associated with trochlear nerve damage.
During the examination, the healthcare professional will also inquire about the patient’s medical history. This includes asking about any previous trauma or surgeries that may have affected the eye or surrounding structures. Additionally, they will explore if there are any underlying medical conditions that could potentially contribute to the nerve damage.
Imaging Techniques
In some cases, the healthcare professional may recommend additional imaging techniques to further investigate the trochlear nerve and surrounding structures. Magnetic resonance imaging (MRI) and computed tomography (CT) scans are commonly used for this purpose. These imaging modalities provide detailed images of the brain, skull, and eye structures, allowing the healthcare professional to identify any structural abnormalities or lesions that may be affecting the trochlear nerve.
By utilizing MRI or CT scans, the healthcare professional can obtain a more comprehensive understanding of the patient’s condition. These imaging techniques can reveal important information about the location, size, and extent of any potential damage to the trochlear nerve. This, in turn, aids in making an accurate diagnosis and determining the most appropriate course of treatment.
Neurological Tests
In addition to clinical examination and imaging techniques, specialized neurological tests may also be conducted to assess the function and integrity of the trochlear nerve. These tests are typically performed by neurologists or ophthalmologists who have expertise in neurological disorders.
One common test used to evaluate the trochlear nerve is nerve conduction studies. This involves the placement of electrodes on the skin near the eye, which measure the electrical signals transmitted by the nerve. By analyzing these signals, the healthcare professional can determine if there are any abnormalities or disruptions in the nerve’s function.
Electrodiagnostic testing is another technique that may be employed. This involves the use of small needles inserted into the muscles surrounding the eye. The needles record the electrical activity of the muscles, providing valuable information about the trochlear nerve’s connection to these muscles.
Interpreting the results of these neurological tests requires specialized knowledge and expertise. Therefore, it is essential to consult with a neurologist or ophthalmologist who has experience in diagnosing and treating neurological disorders. Their expertise ensures that the test results are accurately interpreted and that the most appropriate treatment plan is recommended.
Treatment Options for Trochlear Nerve Damage
Medication and Drug Therapy
In some cases, medication may be prescribed to manage symptoms associated with trochlear nerve damage. Depending on the specific situation and symptoms, these medications may include pain relievers, muscle relaxants, or medications targeted at addressing any underlying neurological conditions contributing to the nerve damage. It is crucial to discuss the risks and benefits of medications with a qualified healthcare professional.
Physical Therapy and Rehabilitation
Physical therapy and rehabilitation can be beneficial in improving eye movement coordination and reducing the impact of trochlear nerve damage on daily activities. A trained therapist can guide the affected individual through specific exercises and techniques that help strengthen the eye muscles and promote effective eye movements. Compliance with the prescribed therapy regimen is essential to achieve optimal results.
Surgical Interventions
In severe cases or when conservative measures fail to provide adequate relief, surgical interventions may be considered. The specific surgical procedure will depend on the underlying cause of the nerve damage. This may involve repairing or repositioning the trochlear nerve, removing any compressive lesions, or addressing associated eye muscle abnormalities. It is important to consult with a qualified ophthalmologist or neurosurgeon to assess the feasibility and potential risks of surgery.
Prognosis and Recovery from Trochlear Nerve Damage
Factors Influencing Recovery
The prognosis for trochlear nerve damage varies depending on the underlying cause, extent of the damage, and individual factors. In cases of mild nerve damage or when the nerve undergoes natural healing, spontaneous recovery may occur over time. However, severe or long-standing nerve damage may have a more guarded prognosis and may require ongoing management to mitigate symptoms and improve functionality.
Coping with Long-Term Effects
Living with trochlear nerve damage can be challenging, especially when facing long-term effects. It is crucial to seek support from healthcare professionals, local support groups, or online resources that provide information and guidance on coping strategies, assistive devices, and adaptive techniques that can help enhance quality of life and promote independence.
Preventing Further Damage
Preventing further damage to the trochlear nerve involves being cautious and taking necessary precautions to minimize the risk of trauma or injury to the head or eye region. This may include wearing appropriate protective gear during sports or avoiding activities that pose a high risk of head or eye injuries. Regular eye examinations and maintaining overall health can also contribute to early detection and management of potential complications.
Conclusion: Living with Trochlear Nerve Damage
Impact on Daily Life
Trochlear nerve damage can significantly impact an individual’s daily life, affecting their ability to perform various tasks that require accurate eye movement and coordination. It may limit career choices and recreational activities and can cause emotional distress. Seeking professional help and support from loved ones can play a crucial role in adapting to the challenges associated with trochlear nerve damage.
Support and Resources
Various support resources and organizations exist to provide guidance and assistance to individuals dealing with trochlear nerve damage. Support groups, online forums, and healthcare professionals experienced in treating neuro-ophthalmic conditions can offer valuable insights, support, and information regarding coping strategies, management options, and available assistive technologies.
Future Research Directions
Ongoing research in the field of neurology and ophthalmology continues to shed light on the mechanisms underlying trochlear nerve damage and potential therapeutic avenues. Research efforts aim to develop innovative treatments, improve diagnostic accuracy, and enhance overall patient outcomes. Individuals affected by trochlear nerve damage may have opportunities to participate in clinical trials or contribute to the advancement of knowledge in this area.
In conclusion, trochlear nerve damage can have profound effects on eye movement coordination and visual function. Seeking early medical attention and prompt diagnosis are essential in managing this condition effectively. While the road to recovery may pose challenges, appropriate treatment options, support resources, and a positive mindset can help individuals adapt and lead fulfilling lives.