The trochlear nerve is one of the twelve cranial nerves that emerge directly from the brain. It is responsible for the movement of the superior oblique muscle in the eye, which is crucial for proper visual coordination and depth perception. Understanding the anatomy and function of the trochlear nerve is essential for comprehending its role in various bodily functions and potential disorders that can arise.
Understanding the Trochlear Nerve
Anatomy of the Trochlear Nerve
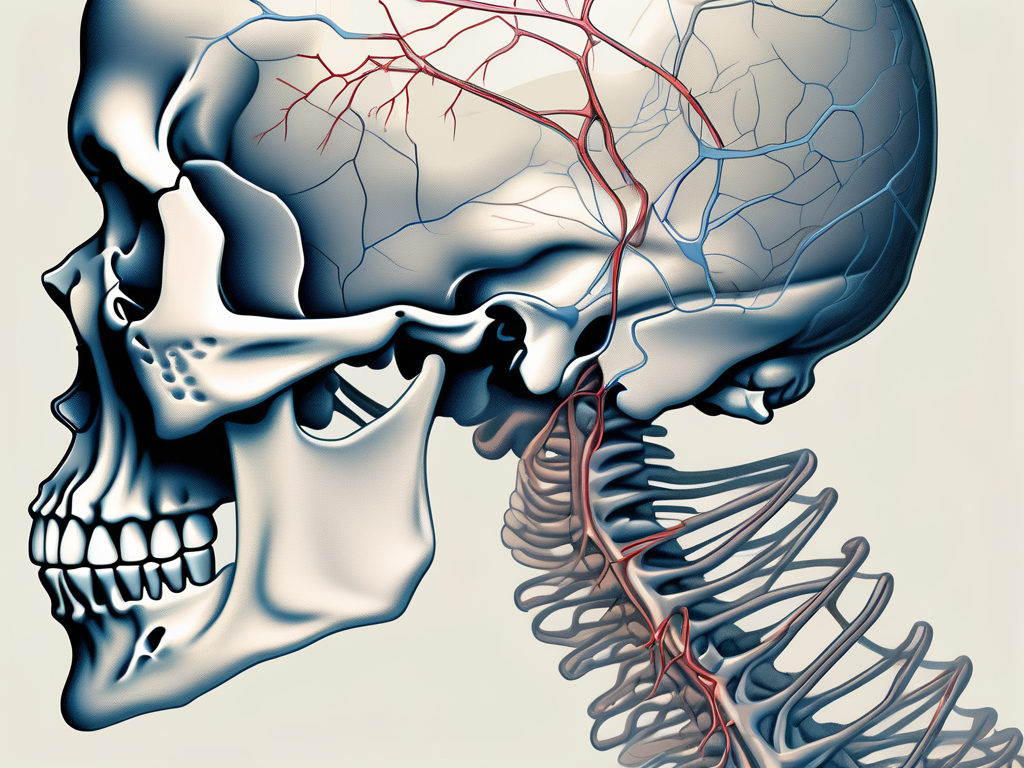
The trochlear nerve, also known as cranial nerve IV, is the smallest of the cranial nerves in terms of the number of axons it contains. It originates from the dorsal aspect of the midbrain, specifically from the trochlear nucleus. The trochlear nucleus is located in the tegmentum of the midbrain, just below the cerebral aqueduct.
Unlike most other cranial nerves, the trochlear nerve decussates or crosses to the contralateral side of the brainstem. This unique anatomical feature allows for precise coordination of eye movements. After crossing, the axons of the trochlear nerve wrap around the brainstem, forming a distinct loop-like structure.
The trochlear nerve exits the skull through a unique anatomical structure known as the superior orbital fissure. This fissure is a narrow opening located in the posterior part of the orbit, between the greater and lesser wings of the sphenoid bone. It serves as a passageway for several structures, including the trochlear nerve, as they travel from the cranial cavity to the orbit.
Once the trochlear nerve exits the skull, it travels along the lateral wall of the cavernous sinus, a large venous channel located behind the eye. The cavernous sinus contains multiple important structures, including other cranial nerves and blood vessels. The trochlear nerve shares this space with these structures, highlighting the intricate nature of the cranial anatomy.
Continuing its course towards the superior oblique muscle, the trochlear nerve sends out branches that innervate this muscle. The superior oblique muscle is one of the extraocular muscles responsible for eye movement. It originates from the back of the orbit and attaches to the top of the eye. The trochlear nerve’s selective innervation of the superior oblique muscle enables fine-tuned control over the eye’s movements, allowing for precise adjustments and coordination.
Function of the Trochlear Nerve
The primary function of the trochlear nerve is to control the superior oblique muscle in the eye. This muscle plays a significant role in eye movement, especially when it comes to the rotational component of vision and maintaining proper alignment of the eyes. The superior oblique muscle helps to rotate the eye downward and inward, allowing us to look down and towards the midline.
Through its innervation of the superior oblique muscle, the trochlear nerve enables us to perceive depth and adjust our visual focus accurately. This is particularly important in tasks that require precise hand-eye coordination, such as threading a needle or catching a ball.
Damage to the trochlear nerve can result in various visual disturbances, such as double vision (diplopia), difficulty looking downward, and problems with vertical eye movements. These symptoms can significantly impact daily activities and quality of life. If you are experiencing any of these symptoms, it is crucial to seek medical advice promptly to determine the underlying cause and appropriate treatment.
The Path of the Trochlear Nerve
Origin of the Trochlear Nerve
The trochlear nerve, also known as the fourth cranial nerve, has a fascinating journey within the human body. Its roots originate from the trochlear nucleus, a vital structure located in the midbrain region. These roots emerge from the dorsal surface of the brainstem, close to the midline.
From its origin, the trochlear nerve fibers embark on a remarkable adventure. They travel dorsally and decussate, meaning they cross over to the opposite side of the brain. This crossing of fibers is a unique characteristic that distinguishes the trochlear nerve from other cranial nerves. It is an essential step that allows for the appropriate innervation of the contralateral superior oblique muscle, a muscle responsible for certain eye movements.
Understanding the intricate path of the trochlear nerve is crucial in comprehending the complexity of the human visual system.
Course of the Trochlear Nerve through the Brain
After crossing to the contralateral side, the trochlear nerve fibers continue their journey, wrapping around the brainstem. They initially travel along the cerebral peduncle, one of the prominent structures on the ventral side of the midbrain.
As the trochlear nerve continues its path, it reaches the posterior aspect of the midbrain, where it encounters various structures and landmarks. Eventually, it enters the cavernous sinus, a venous channel located towards the middle cranial fossa. This intricate network of veins provides a conduit for the trochlear nerve, allowing it to navigate through the skull.
Within the cavernous sinus, the trochlear nerve proceeds along the lateral wall, accompanied by other cranial nerves and blood vessels. This close proximity to other vital structures highlights the interconnected nature of the human anatomy.
From the cavernous sinus, the trochlear nerve embarks on its final leg of the journey. It passes through a bony cleft known as the superior orbital fissure, a crucial anatomical landmark. This fissure marks the nerve’s exit point from the skull, allowing it to reach its destination – the superior oblique muscle located within the orbit.
The intricate path of the trochlear nerve showcases the precision and complexity of the human body. Its role in coordinating precise eye movements is vital for maintaining proper visual function.
The Trochlear Nerve and the Skull
The Trochlear Nerve’s Exit Point from the Skull
The trochlear nerve exits the skull through the superior orbital fissure, a narrow opening located in the sphenoid bone. It is situated in the posterior part of the orbit, close to the optic canal and the common tendinous ring.
The superior orbital fissure, with its strategic location, serves as a gateway for the trochlear nerve to venture into the orbit. This nerve, also known as the fourth cranial nerve, plays a vital role in eye movement and coordination. Its exit point from the skull marks the beginning of its journey towards the superior oblique muscle.
Once the trochlear nerve passes through the superior orbital fissure, it enters the orbit and courses along the superior oblique muscle. This muscle, one of the six extraocular muscles, enables the eye to rotate downward and outward, contributing to gaze stability and accurate alignment.
The intricate interplay between the trochlear nerve and the superior oblique muscle allows for precise control of eye movements. This coordination is essential for activities such as reading, driving, and tracking moving objects. Without the trochlear nerve’s proper functioning, these tasks would become challenging and visually disorienting.
Significance of the Trochlear Nerve’s Exit Point
The exit point of the trochlear nerve from the skull is crucial for its proper functioning and prevention of damage. The superior orbital fissure provides a protective passage for the nerve, ensuring its safe course towards the target muscle.
However, certain conditions or injuries can compromise the integrity of the superior orbital fissure and affect the trochlear nerve’s normal function. Traumatic injuries, such as fractures to the skull or orbital bones, can disrupt the pathway of the nerve, leading to various visual disturbances.
Infections, such as sinusitis or orbital cellulitis, can also pose a threat to the trochlear nerve’s exit point. The inflammation and swelling associated with these conditions can exert pressure on the nerve, impeding its ability to transmit signals effectively.
Tumors, although relatively rare, can also impact the trochlear nerve’s exit point. Depending on their location and size, tumors can compress the superior orbital fissure, causing compression of the nerve and subsequent visual impairments.
Furthermore, anatomical variations in the skull and orbit can contribute to the vulnerability of the trochlear nerve. Some individuals may have a narrower or more constricted superior orbital fissure, predisposing them to nerve compression and potential complications.
If you experience any unusual symptoms, such as double vision, difficulty moving your eyes, or pain around the eye area, it is vital to consult with a healthcare professional. Prompt evaluation and diagnosis can help identify any trochlear nerve involvement and guide appropriate treatment options.
In conclusion, the trochlear nerve’s exit point from the skull through the superior orbital fissure is a critical juncture in its journey towards controlling eye movement. Understanding the significance of this exit point and the potential challenges it may face can aid in the early detection and management of trochlear nerve-related conditions.
Disorders Related to the Trochlear Nerve
The trochlear nerve, also known as the fourth cranial nerve, plays a crucial role in eye movement. When this nerve is damaged, it can lead to various disorders and symptoms that can significantly impact a person’s vision and overall quality of life.
Symptoms of Trochlear Nerve Damage
Damage to the trochlear nerve can result from various causes, including trauma, infections, or underlying medical conditions. Depending on the severity and location of the damage, the symptoms can vary but often include:
- Double vision (diplopia), typically when looking downward or inwards
- Vertical misalignment of the eyes (hypertropia)
- Difficulty with downward eye movement
- Squinting or tilting of the head to compensate for visual disturbances
- Eye strain or headaches due to the extra effort required to maintain proper eye alignment
Double vision, also known as diplopia, is a common symptom of trochlear nerve damage. It occurs when the eyes are unable to align properly, resulting in two images instead of one. This visual disturbance can make it challenging to perform daily activities such as reading, driving, or even walking.
Vertical misalignment of the eyes, known as hypertropia, is another common symptom of trochlear nerve damage. It causes one eye to be higher than the other, leading to an uneven gaze. This can affect depth perception and make it difficult to focus on objects at different distances.
The trochlear nerve is responsible for controlling the downward movement of the eyes. When damaged, it can result in difficulty looking down, making it challenging to navigate stairs, read, or perform tasks that require looking at objects located below eye level.
To compensate for the visual disturbances caused by trochlear nerve damage, individuals may develop coping mechanisms such as squinting or tilting their head. These actions can provide temporary relief by altering the angle of vision, but they are not a long-term solution and can lead to discomfort and strain.
Individuals with trochlear nerve damage often experience eye strain and headaches due to the extra effort required to maintain proper eye alignment. The eyes may constantly be working harder to compensate for the misalignment, leading to fatigue and discomfort.
If you experience any of these symptoms, it is essential to seek medical evaluation to determine the cause and appropriate treatment options.
Treatment Options for Trochlear Nerve Disorders
The management of trochlear nerve disorders depends greatly on the underlying cause and the severity of symptoms. In many cases, the primary goal is to address the root cause of the damage and provide supportive care to alleviate symptoms and improve functionality.
Treatment options may include:
- Medications to manage inflammation, infections, or underlying medical conditions
- Eye patching or prism glasses to alleviate diplopia and improve eye alignment
- Vision therapy exercises to enhance eye coordination and muscle strength
- Surgical interventions, in rare cases, to correct structural abnormalities or relieve nerve compression
In cases where trochlear nerve damage is caused by inflammation, infections, or underlying medical conditions, medications may be prescribed to address these issues. By treating the underlying cause, it is possible to reduce the impact on the trochlear nerve and improve symptoms.
Eye patching or prism glasses can be used to alleviate diplopia and improve eye alignment. By covering one eye or using specially designed glasses, the brain can be trained to suppress the image from the misaligned eye, reducing double vision and improving overall visual perception.
Vision therapy exercises are often recommended to enhance eye coordination and muscle strength. These exercises can help train the eyes to work together, improving eye alignment and reducing the strain on the trochlear nerve. Vision therapists work closely with patients to develop personalized exercise programs tailored to their specific needs.
In rare cases where trochlear nerve damage is caused by structural abnormalities or nerve compression, surgical interventions may be necessary. These procedures aim to correct the underlying issue, relieving pressure on the nerve and restoring proper eye movement.
It is crucial to consult with a healthcare professional experienced in neurology or ophthalmology to determine the most appropriate treatment plan for your specific case. They can provide individualized guidance and monitor your progress throughout the recovery process.
Frequently Asked Questions about the Trochlear Nerve
How to Keep the Trochlear Nerve Healthy
Maintaining good overall health is crucial for supporting the well-being of the trochlear nerve and the entire nervous system. While specific methods to target the trochlear nerve directly are limited, incorporating healthy habits into your lifestyle can contribute to optimal nerve function. Here are a few tips:
- Eat a balanced diet rich in essential nutrients, including vitamins and minerals.
- Engage in regular exercise to promote blood flow and overall well-being.
- Protect your eyes from injuries by using appropriate safety measures such as goggles or protective eyewear.
- Take breaks when engaging in activities that require prolonged focus or eye strain, such as screen time or reading.
- Visit an optometrist or ophthalmologist regularly for comprehensive eye examinations to detect and address any potential issues early on.
Remember that these suggestions are general lifestyle recommendations and may not specifically target the trochlear nerve. If you have concerns about your trochlear nerve or experience any related symptoms, it is crucial to consult with a qualified healthcare professional.
What Happens if the Trochlear Nerve is Damaged?
Damage to the trochlear nerve can lead to various visual disturbances and interfere with the coordinated movement of the eyes. The specific effects of trochlear nerve damage may vary depending on the severity and location of the injury.
If the trochlear nerve is damaged, symptoms can include double vision, difficulty looking downward, problems with vertical eye movements, eye strain, and headaches. It is important to seek medical evaluation if you experience any of these symptoms, as prompt diagnosis and appropriate treatment can help manage and improve the condition.
Conclusion
The exit point of the trochlear nerve from the skull plays a crucial role in its proper functioning and protection from potential damage. Understanding the anatomy and function of the trochlear nerve provides insight into its essential role in coordinating eye movements and maintaining visual stability.
Disorders related to the trochlear nerve can manifest in various ways, including double vision, misalignment of the eyes, and difficulty with eye movements. Seeking medical evaluation and following the guidance of healthcare professionals can help diagnose and manage these conditions effectively.
To ensure the overall health of the trochlear nerve and the visual system as a whole, maintaining a healthy lifestyle, protecting the eyes, and seeking regular eye examinations are vital. Remember, any concerns regarding the trochlear nerve or visual impairments should be addressed by healthcare professionals experienced in neurology or ophthalmology.